The field of behavioral economics has already been applied to address one facet of the opioid epidemic: most recently, the insights from the behavioral sciences have been used to reduce opioid prescribing in EDs. This is despite evidence that shows that emergency physicians are responsible for just a small percentage of the overall opioid prescriptions written nationally. For example, in 2012 less than 5% of all opioid pills prescribed originated from emergency room doctors. In a recent study, Dr. Doctor et al of the USC Price School of Public Policy found that when emergency physicians have learned in a letter from the medical examiner that one of their patients has suffered a fatal opioid overdose, they reduced the amount of opioids they prescribed by almost 10% over the next three months. Another study from the University of Pennsylvania sought to use new default options as a nudge in electronic health records (EHRs) in an effort to decrease the number of opioid pills that physicians prescribe.
While efforts to reduce the risk of unnecessary exposure to opioid prescriptions are certainly a part of the solution, more can be done to leverage behavioral science to change provider behavior around prescribing life saving MAT. We sought to leverage the field of behavioral economics to support providers caring for patients struggling with OUD in an ED at an academic medical center by first understanding the pre-existing behavioral challenges related to prescribing MAT in EDs.
Barriers and Nudges
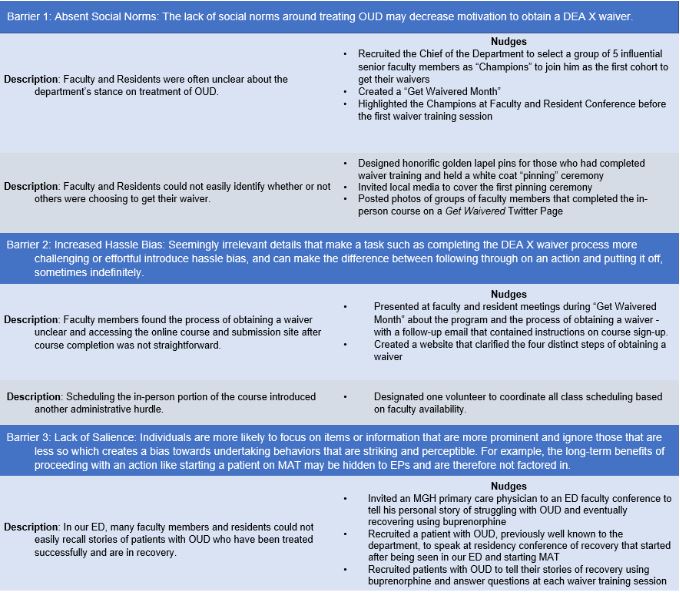
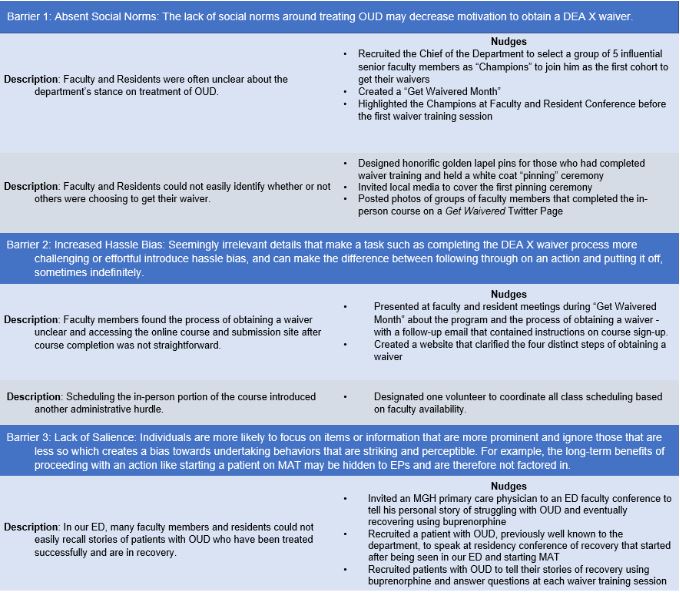
We uncovered three key behavioral barriers that impeded completion of the DEA X waiver process for our faculty and residents. Our team of behavioral economists worked to intuit the key psychological or situational factors behind each of these barriers and developed approaches that could be used to address them. These may be common themes and relevant approaches for stakeholders interested in making similar changes at their institutions as well.
Barrier 1: Absent Social Norm
Behavioral economics defines social norms as the values, actions, and expectations of a culture or group. They offer, often implicit, guides to our behavior and, in particular, descriptive norms make people aware of what “most other people are doing”. These norms can reinforce and amplify an individual’s underlying motivations. The lack of consistent social norms around treating OUD and subsequently getting a waiver undercut the motivation of many attendings in our department to obtain a waiver. We targeted this barrier using six specific nudges including recruiting influential faculty members to be the first group of those waivered, creating a ‘Get Waivered’ Month, and holding a white coat pinning ceremony which was covered in a local news story and social media for those who had completed their waiver process as shown in figure 1.
Barrier 2: Hassle Bias in Obtaining a Waiver
Seemingly irrelevant details that make a task more effortful introduce hassle bias, and can make the difference between following through on an action and putting it off, sometimes indefinitely. Our group identified that many of the behaviors required to obtain their a DEA-X waiver introduced hassle bias including: accessing the online course and submission site after course completion and scheduling the in-person portion of the course. We targeted this barrier using three specific nudges including coordinating all schedules for interested participants, creating an easy to follow website, and presenting about the waivering process at resident and faculty conferences as shown on figure 1.
Barrier 3: Lack of Salience in Treating OUD
Salience refers to the fact that individuals are more likely to focus on items or information that are more prominent and ignore those that are less so. This creates a bias towards undertaking behaviors that are striking and perceptible. In the ED, the long-term benefits of proceeding with an action like starting a patient on MAT may be hidden and are therefore not always factored in at the time of decision making. Moreover, an emergency physician may be hard pressed in daily practice to remember stories of patients with OUD who have been treated successfully and are in recovery. Thus, because they are not regularly exposed to positive outcomes from OUD treatment, emergency physicians may come to develop an impression that patients cannot be treated effectively or recover. This worldview may alter their willingness to expend the effort to undergo extra training to obtain a DEA-X waiver. Making the benefits of our actions in treating patients with OUD more salient through vivid stories provides an opportunity to increase the motivation to follow through on obtaining a waiver. We targeted this barrier using three specific nudges around sharing in-person patient stories, including of physicians with OUD, who used MAT to enter into and stay in recovery as shown on figure 1.