The fight against opioid use disorder (OUD) in rural areas is vital to the hopeful end of this epidemic in the United States. Individuals are more likely to die from an overdose in a rural setting, as opposed to an urban setting.5 What is most striking however is that there are more people struggling with OUD in urban areas. This high mortality rate is likely due to insufficient transportation to and availability of treatment facilities. If nurse practitioners (NPs), and physician assistants (PAs) obtain federal waivers, more individuals may have access to treatment.The ability for mid level providers to be able to initiate buprenorphine treatment in primary care settings, could reduce the fears and stigmas associated with getting treatment for OUD.
In 2016, the Comprehensive Addiction and Recovery Act (CARA) allowed NPs and PAs to obtain DEA-X waiver to prescribe buprenorphine, a medication that is effective in treating OUD. Effectively between 2016 and 2019 the number of waivered PAs and NPs rose by more than 50% in rural U.S. This is especially important because over the past few years there has been a trend of physicians moving out of rural neighborhoods, and increased presence of mid level providers in practice.7 By encouraging NPs and PAs to receive a waiver this may help lighten the burden in counties where there are very few providers with DEA-X waiver.
In a 12 month study done in 2019, less than 35% of adults in the U.S. struggling with OUD were found to be receiving treatment.6 One reason the level of treatment is this low may be due to the stigma3 associated. If patients have the opportunity to see a primary care provider, with whom they already have established relationships, the patient might feel more comfortable with discussing treatment plans.
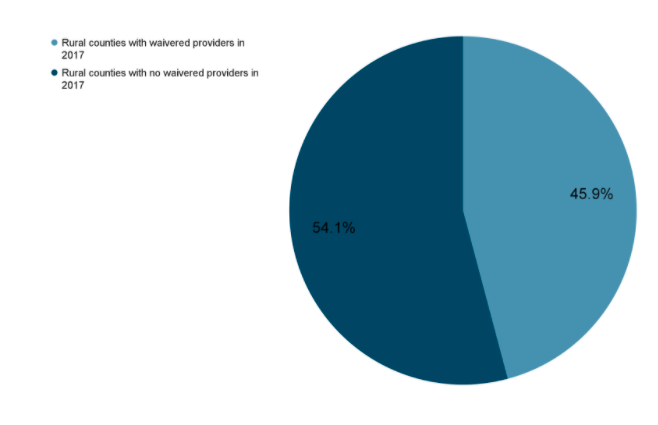
Despite the growth seen of newly waivered providers, there are still a significant number of counties with no waivered NPs and PAs. The majority of these providers are found in the Eastern and Western coasts of the U.S.3 In March 2019, 52% of rural counties had 1 or more waivered NPs or PAs. It is easy to sign up, and the process can be completed within 8 minutes. To register for training in your area click here.
______________________________
- Andrilla, C. H., Patterson, D. G., Moore, T. E., Coulthard, C., & Larson, E. H. (2018). Projected contributions of nurse practitioners and physicians assistant to Buprenorphine treatment services for opioid use disorder in rural areas. Medical Care Research and Review, 77(2), 208-216. doi:10.1177/1077558718793070
- Andrilla, C. H., Moore, T. E., Patterson, D. G., & Larson, E. H. (2018). Geographic Distribution of Providers With a DEA Waiver to Prescribe Buprenorphine for the Treatment of Opioid Use Disorder: A 5-Year Update. The Journal of Rural Health, 35(1), 108-112. doi:10.1111/jrh.12307
- Barnett, M. L., Lee, D., & Frank, R. G. (2019). In rural areas, buprenorphine waiver adoption since 2017 driven by nurse practitioners and physician assistants. Health Affairs, 38(12), 2048-2056.
- Jackson, H. J., & Lopez, C. M. (2018). Utilization of the nurse practitioner role to combat the opioid crisis. The Journal for Nurse Practitioners, 14(10). doi:10.1016/j.nurpra.2018.08.016
- Mack, K. A., Jones, C. M., & Ballesteros, M. F. (2017). Illicit drug use, illicit drug use disorders, and drug overdose deaths in Metropolitan AND nonmetropolitan areas — United States. MMWR. Surveillance Summaries, 66(19), 1-12. doi:10.15585/mmwr.ss6619a1
- U.S. News & World Report. (n.d.). What to Do When There Are No Primary Care Physicians Accepting Patients Near You. U.S. News & World Report. https://health.usnews.com/health-care/patient-advice/articles/2018-02-12/what-to-do-when-there-are-no-primary-care-physicians-accepting-patients-near-you.